Primary Authors: Jade Deschamps, Vi Dinh; Co-authors: Jessica Ahn, Satchel Genobaga, Annalise Lang, Victor Lee, Reed Krause, Devin Tooma, Seth White. Oversight, Review, and Final Edits by Vi Dinh (POCUS 101 Editor).
Lung ultrasound (also known as chest ultrasound, thoracic ultrasound, and pulmonary ultrasound) is a Point of Care Ultrasound (POCUS) application that can be used to diagnose almost any lung pathology in seconds while outperforming chest x-ray!
After reading this lung ultrasound tutorial you will learn:
- How to perform a Lung Ultrasound Protocol
- Proper Lung Ultrasound Probe Position
- Lung Ultrasound Technique
- What does lung sliding mean
- What do “B-lines” mean
- How to interpret Normal Lung Ultrasound
- All lung ultrasound signs with Examples
- How to diagnose all major lung ultrasound pathology
Editor’s Note: The 6-point lung ultrasound protocol we describe in this post is what is used at our institution and is adapted from Lichtenstein, 2014. We will show you how we label all of the points to make it easy for you to follow. Feel free to adapt or revise the lung ultrasound protocol as you see fit at your institution!
Lung Ultrasound Indications
Lung ultrasound can be used when you are assessing for:
- Shortness of breath
- Pneumonia or other recurring infections
- Cardiogenic pulmonary edema
- Acute Respiratory Distress Syndrome (ARDS)
- COPD/Asthma
- Pneumothorax
The major limitations of lung ultrasound are:
- Subcutaneous emphysema: ultrasound waves can’t pass through the air in the skin to evaluate the lungs
- Patient body habitus: may be difficult to see the lung in severely obese patients
Lung Ultrasound Pre-Exam Preparation
Patient Preparation
- Patient position: the patient may lie supine, lateral decubitus, or sit erect. For this post, we will be having the patient in the supine position.
- If you’re scanning the right lung, you will ask the patient to lift their right arm and place their hand behind their head, and vice versa for the left lung.


Ultrasound Machine Preparation
A common question that comes up is “What ultrasound probe is used for lung ultrasound?” In general, using a curvilinear probe or phased array probe will be just fine. However, if you really want to see the more shallow pleura then you may need to switch to the linear probe.
- Transducer: Curvilinear Ultrasound Probe or Phased Array Probe.
- The linear transducer may be used for shallow imaging to scan the pleura close to the chest wall.
- Preset: Lung or Abdominal
- Machine Placement: Place the machine on the patient’s right side so you can scan with your right hand and manipulate ultrasound buttons with your left hand.

Lung Ultrasound Anatomy
We will be using lung ultrasound to look for pathology that affects the pleura, alveoli, and interstitium.
The parietal pleura interfaces with the visceral pleura, creating a sliding motion as we breathe. We will later discuss how this “lung sliding” motion is a very important finding during an ultrasound because it can rule out disease processes such as pneumothorax.
Alveoli exist in lobules that are subdivided by interlobular septa. The septa anchor into the visceral pleura to stabilize the lobules. When these areas fill with fluid due to consolidation or pulmonary edema, we see various artifacts manifest on ultrasound.
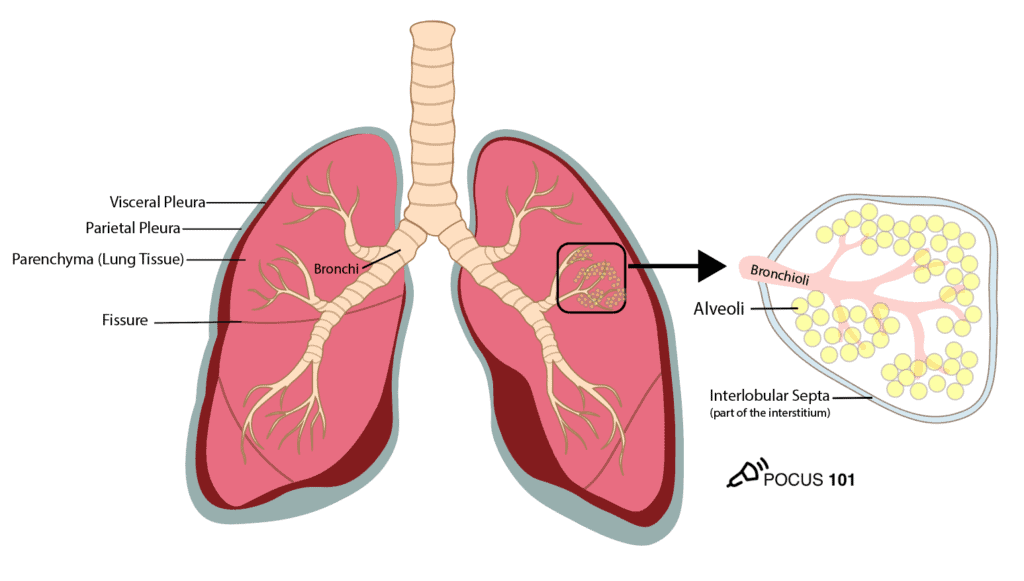
It is important to remember that ultrasound waves are completely scattered and attenuated (absorbed) by the air that fills healthy alveoli. Thus, if the patient has normal lungs, you should not be able to see the texture of the parenchyma (lung tissue) during your scan.
However, in certain pathologies like interstitial lung edema, the accumulated fluid in the interlobular septa results in lung ultrasound artifacts known as “B-lines.” And as lung disease progression worsens further, you may start to even see entire consolidation of the lung on ultrasound. We will discuss this further in the pathology section of this post.
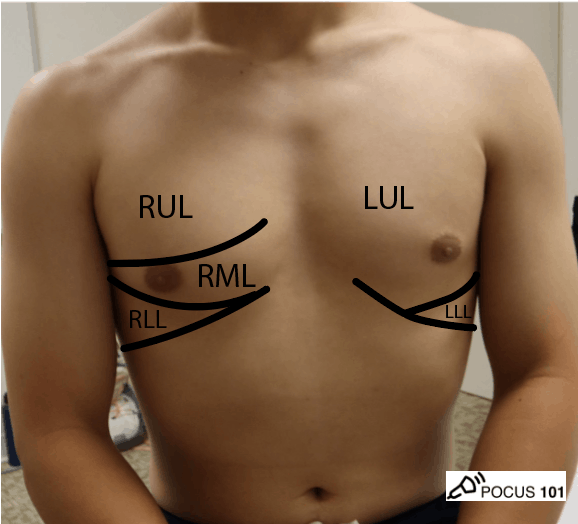
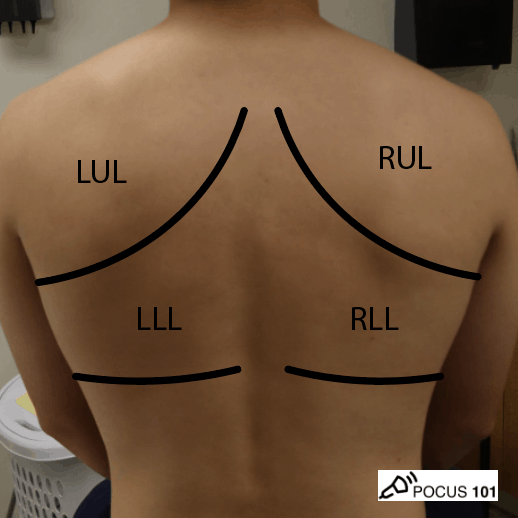
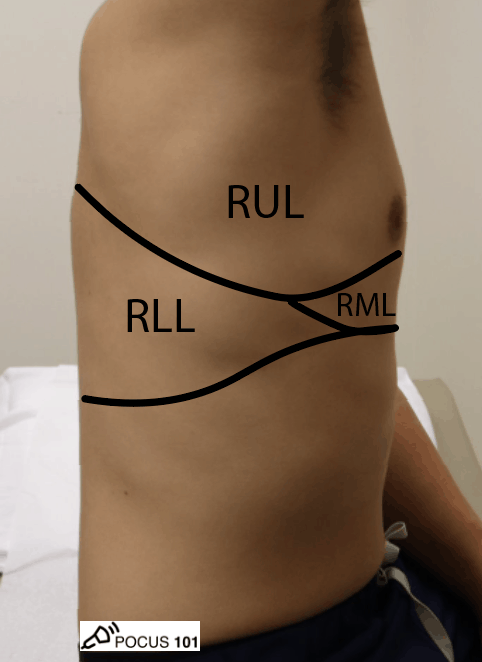
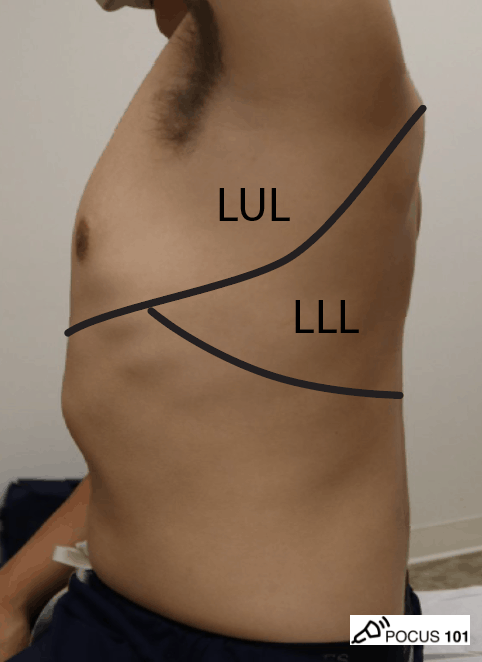
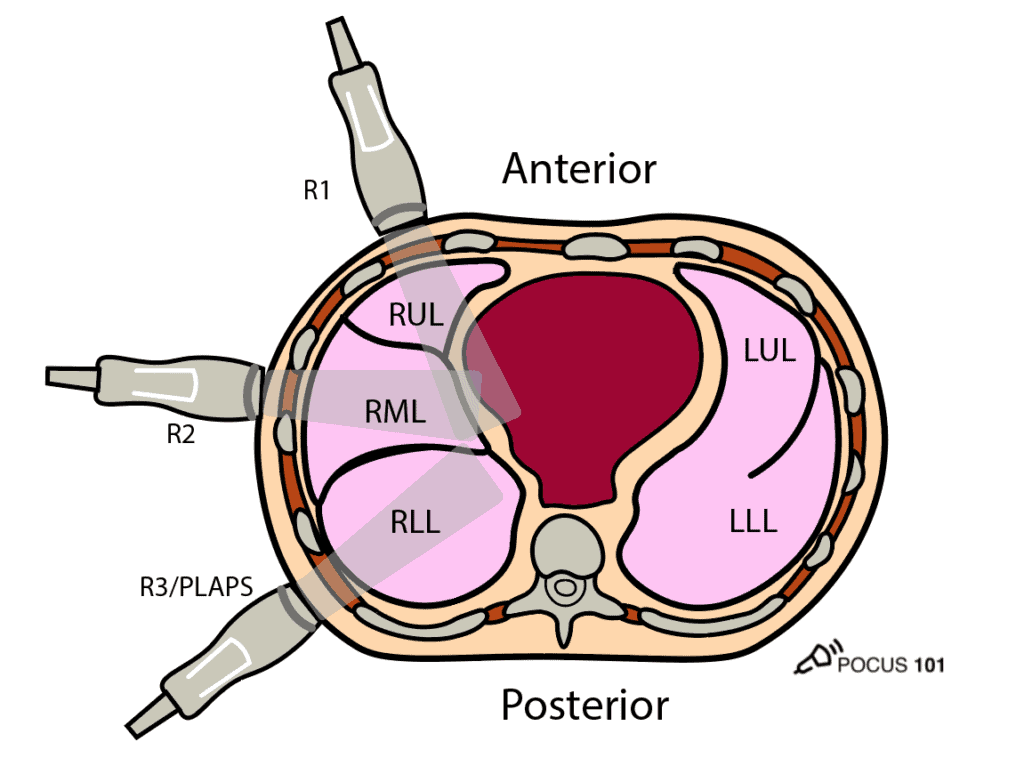
Surface Anatomy of the Lung and Lobes
Here is a quick refresher for lung surface anatomy. Here we are able to see the surface anatomy for the right and left upper lobes, right middle lobe, and left lower lobes. In the next section, we explain the 6 point lung ultrasound exam we use.
Abbreviations: RUL: Right Upper Lobe, RML: Right Middle Lobe, RLL: Right Lower Lobe, LUL: Left Upper Lobe, LLL: Left Lower Lobe
Step-by-Step Lung Ultrasound Protocol
Defining the 6-Point Lung Ultrasound Exam
In general, we recommend a 6-point exam for general lung ultrasound (Lichtenstein, 2014). However, for situations when assessing for COVID-19 or other viral pneumonia, the lung can be affected in a multi-lobar manner and you should consider doing a more extensive 12-point exam which you can read HERE.
In this section, you will learn how to position your probes properly and identify basic structures. We label the 6 lung points at our institution for easy reference and labeling on the ultrasound machines. We refer to these points as R1, R2, R3 for the right lung and L1, L2, L3 for the left lung respectively.
| Probe Position | Lung Field |
| R1 and L1 | Anterior Superior |
| R2 and L2 | Lateral |
| R3 and L3 (PLAPS) | Posterior Inferior |
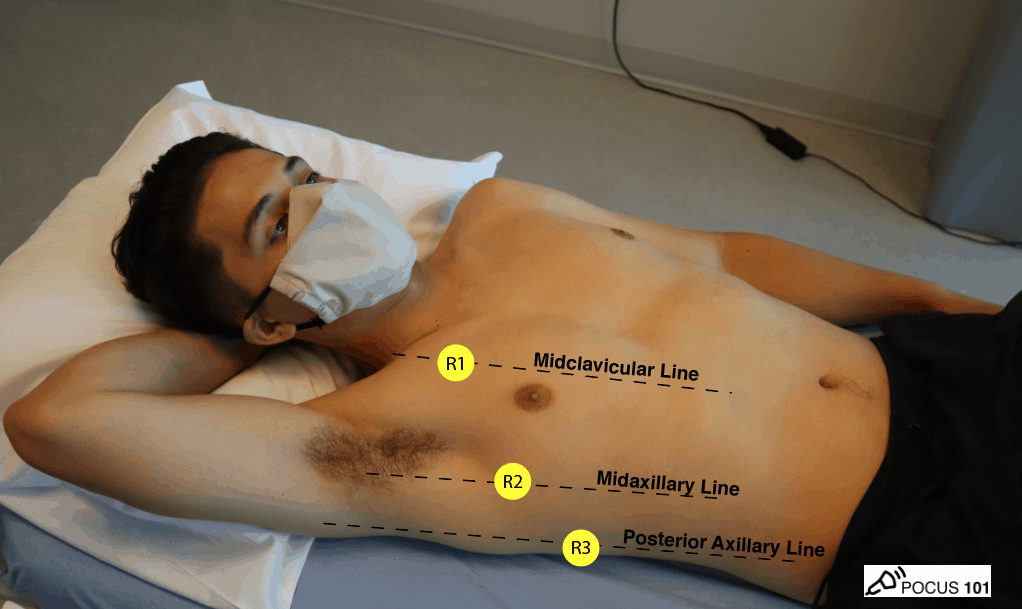
Step 1: LungUltrasound of ANTERIORChest (R1/L1)
Point 1 (R1 and L1) assesses the anterior chest. This point will be most relevant when assessing for pneumothorax and/or interstitial edema.
- Point your indicator towards the patient’s head.
- Place your probe at the mid-clavicular line at the 2nd intercostal space of the right (R1) and left (L1) lungs respectively
- Anchor your probe in the space between two ribs.
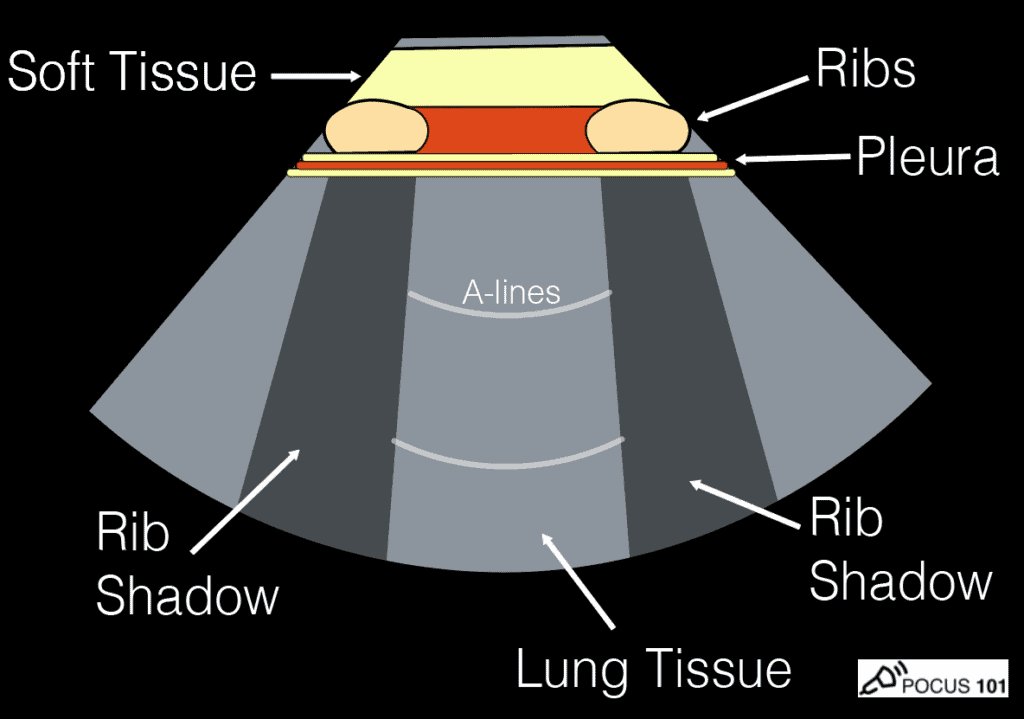
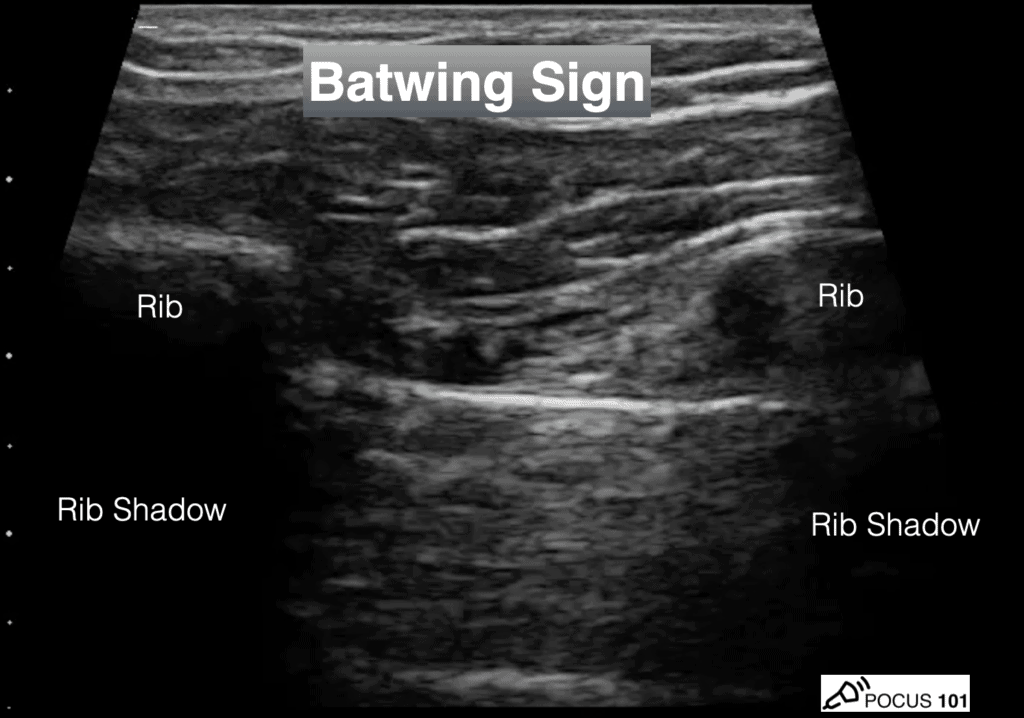
Identify Two Rib Shadows (Batwing Sign)
- The first lung ultrasound finding to confirm you are in the correct position is to look for the two rib shadows or the “Batwing Sign.” This ensures that your probe is in between two ribs.
Identify Lung Sliding
- The next finding you will want to look for is lung sliding.
- Lung sliding is a normal finding where the visceral and parietal pleura slide back and forth on one another as the patient breathes. Some say this looks like tiny “ants marching on a line.”
- This is a simple finding but extremely useful since lung sliding definitely means that the visceral and parietal pleura are next to each other, effectively ruling out pathology such as pneumothorax.
Editor’s Note: Lung sliding can be seen with the phased array and curvilinear ultrasound probes. However it is often times most easily seen with the linear probe given how shallow it is.
Lung Sliding using M-Mode (Optional)
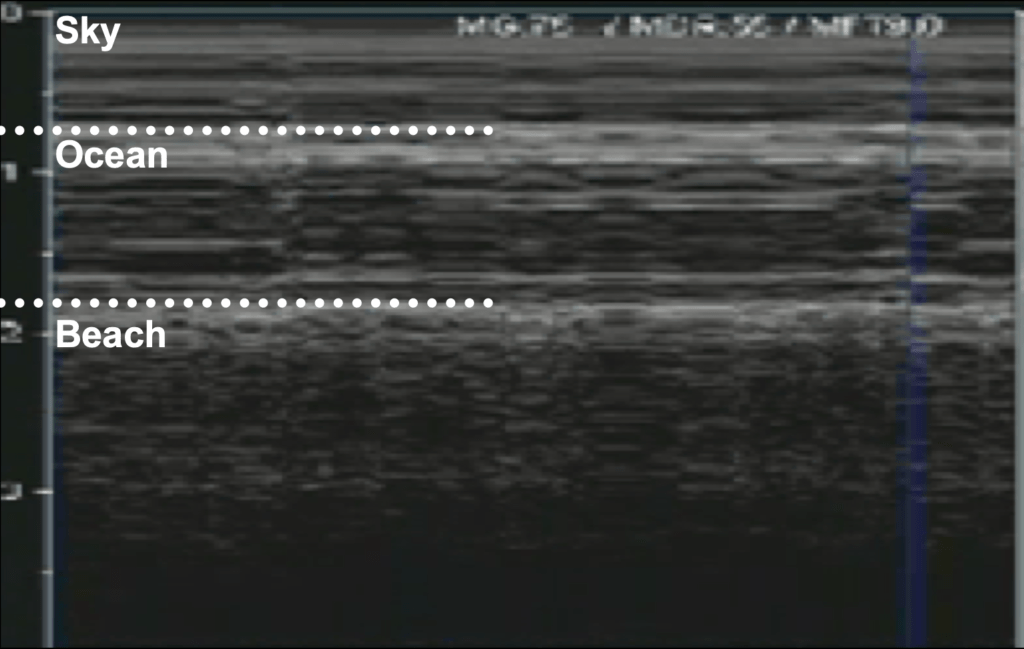
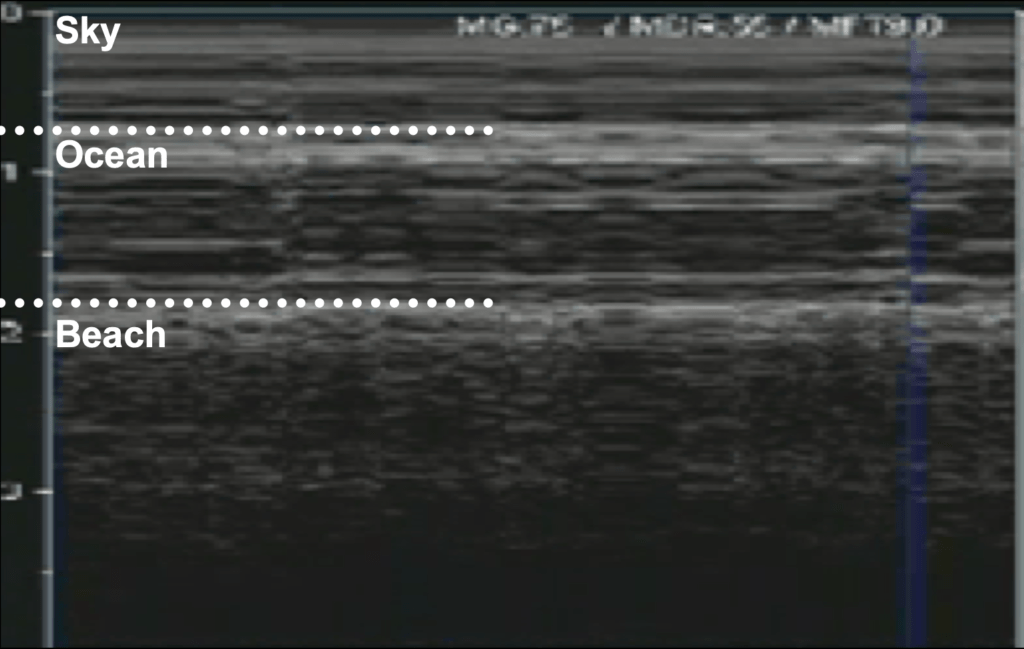
- If lung sliding is not readily apparent, it can be further be evaluated using M-Mode. The goal of M-Mode is to see if the patient has a normal seashore sign.
- Seashore Sign: Sky = Skin/Subcutaneous Tissue, Ocean= Muscle, Beach = Lung sliding motion (sandy appearance)
Here is a quick video on how to use M-mode for lung ultrasound:
Identify A-lines
When you angle your probe perpendicular to the pleura, ultrasound waves reflect off the air from the pleura and the probe surface, producing an image of what looks like pleural lines that lie equidistant to the true pleural line. These reverberation artifacts can continue reflecting back and cause several A-lines to appear before dissipating. (A1 = first A-line seen, A2 = second A-line seen, A3 = third A-line seen)
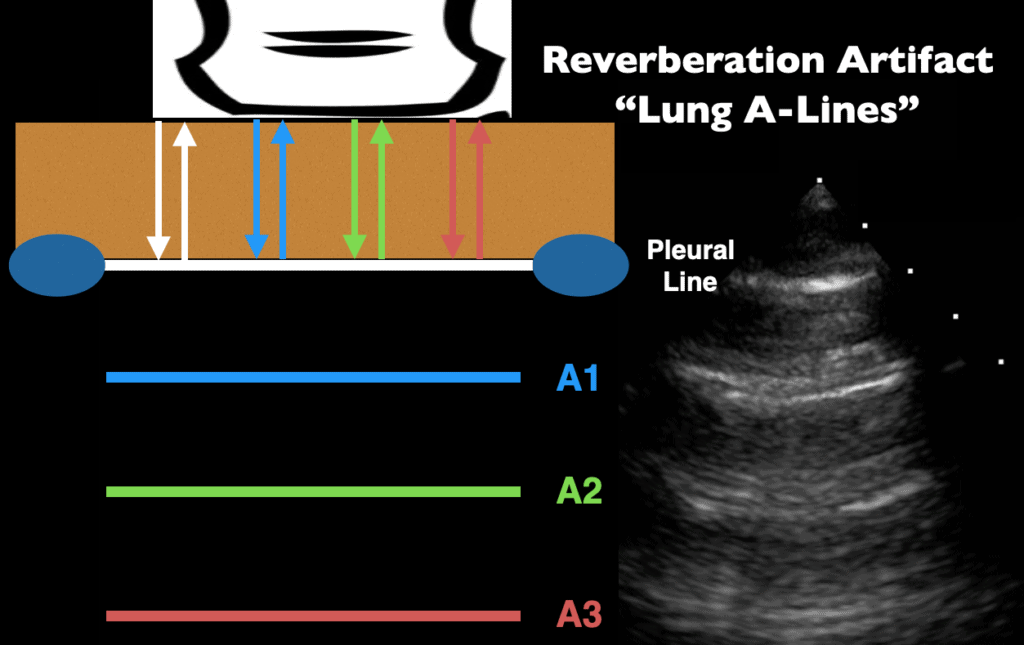
Clinically, A-lines can indicate healthy aeration of the alveoli. However, A-lines can also be seen in cases of pneumothorax since there will be a reflection of air at the parietal pleura. The difference is that you will not see lung sliding in pneumothorax (will discuss this much more in the pathology section below).
Step 2: Lung Ultrasound of LATERAL Chest (R2/L2)
Point 2 (R2 and L2) examines the lateral chest.
- Place your probe at the right (R2) or left (L2) Midaxillary line around the 6-7th intercostal space. This should be just lateral to the nipple line in males.
- Anchor your probe between two ribs, and just like in point 1, look for the batwing sign, lung sliding, and A-lines.

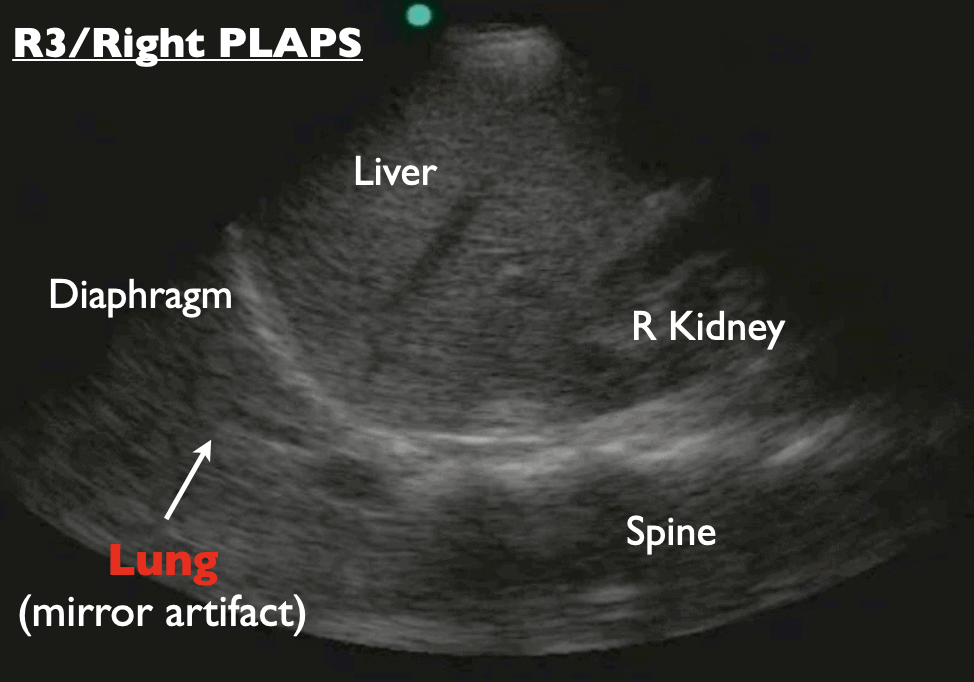
Step 3: Lung Ultrasound of POSTERIORChest (R3/L3-PLAPS)
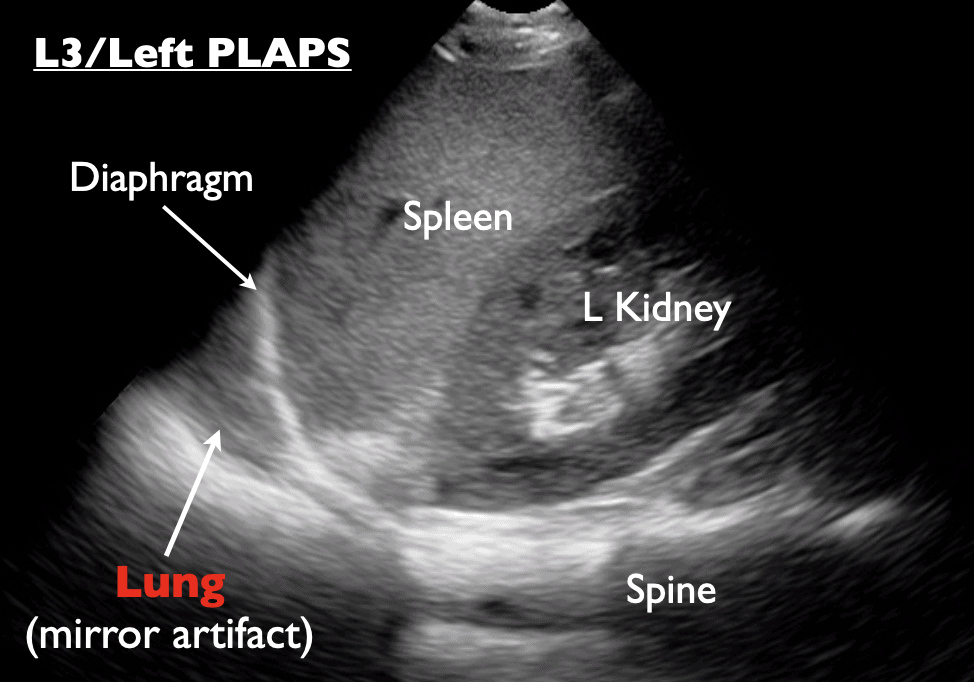
Point 3 (or R3 and L3) assesses the posterior chest. This point is commonly known as the PLAPS point on lung ultrasound (“posterior and/or lateral alveolar and/or pleural syndrome”). The PLAPS will be most relevant for assessing the presence of pleural effusions and consolidations.
- Point your indicator towards the patient’s head.
- Slide the probe under the patient at the PLAPS point at the intersection of the posterior axillary line and a rib space between the 10th and 12th ribs.

- Identify the liver (right side) or spleen (left side), kidney, and diaphragm.
- These organs will come in and out of view when the lung inflates and deflates.
- You should also see the spine, which in healthy lungs, extends up only until the border of the diaphragm. If it extends past the diaphragm called the “spine sign”, you will need to look for a pleural effusion or consolidation which we explain how to do in the pathology section.
Curtain Sign
The curtain sign is seen in healthy and aerated lungs at point 3 (PLAPS position). An aerated lung is like a “curtain” because as it fills with air, it looks like a curtain sweeping down and over the other organs, momentarily obscuring them from view. The diaphragm, liver, or spleen reappear during exhale.
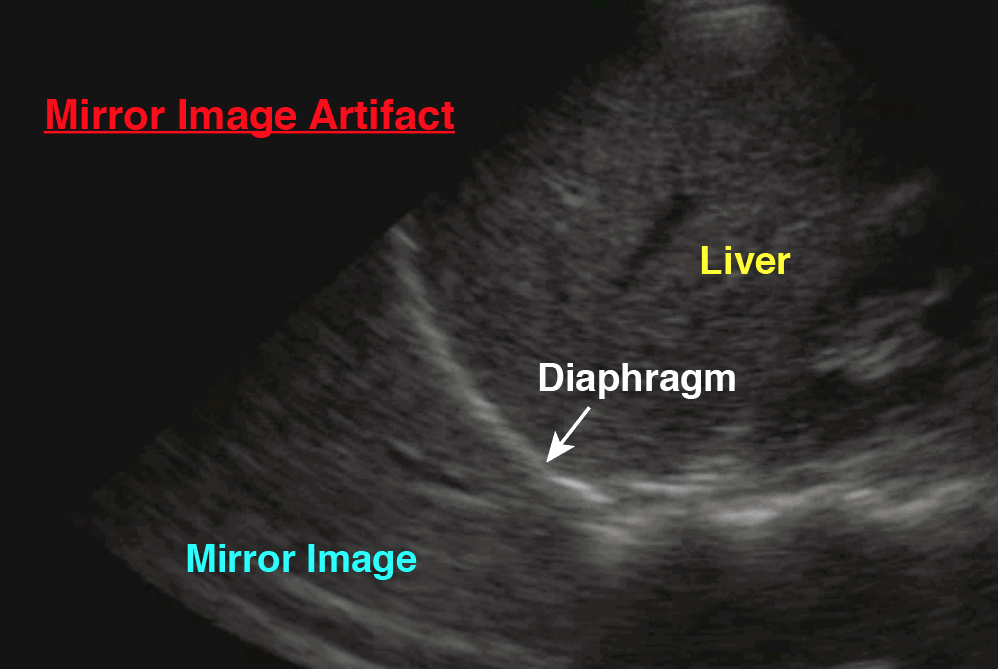
Mirror Image Artifact
Mirror image artifacts are a normal finding that occurs when reflection from a structure creates a false image behind a reflective object, such as the diaphragm, as seen in the image below. This is a normal finding in the PLAPS position.
Lung Ultrasound Video Summary
Lung Ultrasound Signs and Findings
Before we look at specific lung diseases with ultrasound, you will first need to understand the pathological signs and findings of lung ultrasound.
Lung ultrasound pathology profiles such as pneumothorax, pneumonia, cardiogenic pulmonary edema, etc will have a different combination and distribution of these pathological lung ultrasound findings/signs. Once you understand these basic lung ultrasound findings you will be able to interpret just about any lung ultrasound images.
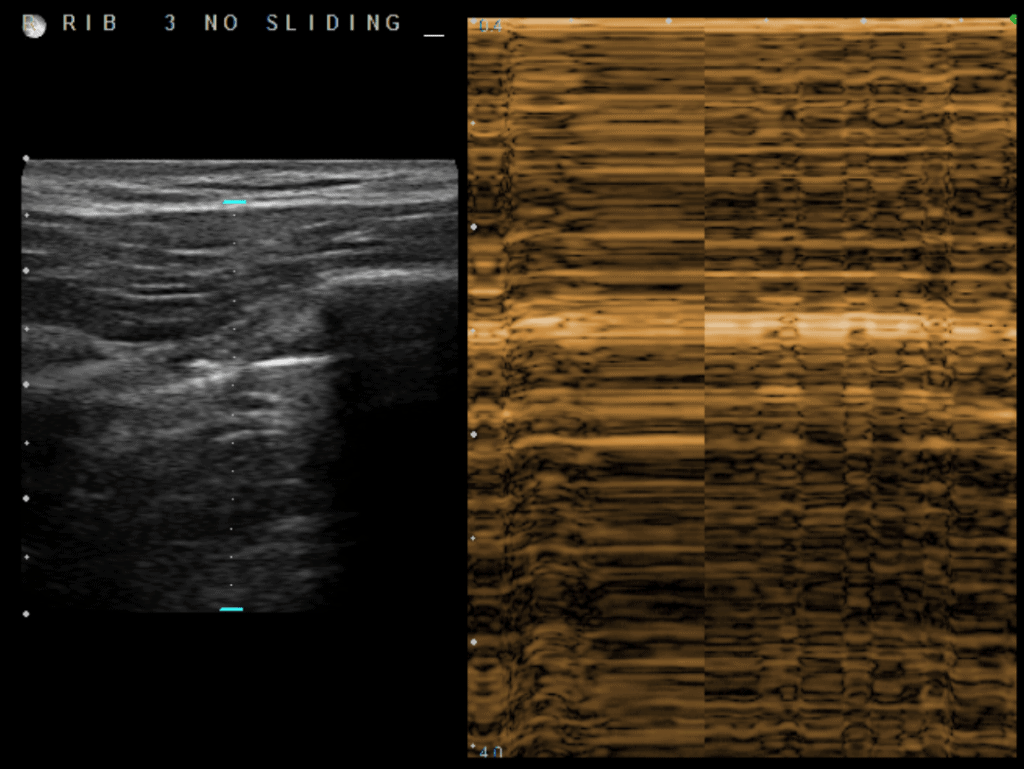
Absent Lung Sliding
Lung sliding may be reduced or absent in a variety of circumstances. There is no lung sliding present when the parietal and visceral pleura become separated by air (pneumothorax) or fluid (pleural effusion). Furthermore, severe COPD or anything that hyperinflates the lungs can markedly reduce pleural sliding.
Absence of lung sliding can be seen using B-mode or using M-mode (stratosphere sign and barcode sign).
The most clinically relevant fact about lung sliding is that if lung sliding is present, you can rule out pneumothorax with 100% sensitivity. On the flip side, the absence of lung sliding can have many causes with pneumothorax being one of them.
Thus, if your patient does not have lung sliding, you must use your patient’s clinical features to consider other causes such as severe consolidation, chemical pleurodesis, acute infectious or inflammatory states, fibrotic lung diseases, acute respiratory distress syndrome, or mainstem intubation.
Interstitial Edema/Syndrome and B-lines
The lung interstitium, or the network of tissue that supports the alveoli and blood vessels, can thicken or fill with fluid.
B-lines form when interlobular septa and lung tissue thicken or fill with fluid. Thus, many clinicians have equated B-lines with “wet lung.” Remember, A-lines are horizontal while B-lines are vertical.
In order to be sure you are seeing B-lines, make sure they have these following qualities (Lichtenstein, et al):
- Appear ray-like, hyperechoic, and vertical.
- Emanate from the pleural line.
- Move with lung sliding.
- Extend to the periphery of the far-field.
- Can be associated with a thickened pleural membrane.
It is worth noting that patients with chronic scarring of their septa from pulmonary fibrosis, old infections, or interstitial lung disease have chronically widened/thickened septa that also create B-lines even without a “wet lung” etiology. Furthermore, lung fissures between the lobes can produce single B-lines, so less than 3 B-lines in a single field of view is generally considered normal.
Confluent B-lines
- As more fluid builds ups, it will become increasingly difficult to differentiate between singular B-lines. Thus, as more and more B-lines converge, they can create an appearance of “Confluent B-lines.”
Consolidations
As even more fluid builds up in the lung, parts of the lung can become completely fluid-filled, leading to consolidation. This is commonly seen in pneumonia. Note that consolidation can also be due to atelectasis from airway obstruction (i.e. mucous plug) or extrinsic compression (i.e. large pleural effusion).
As fluid build-up progresses, your ultrasound findings will progress from multiple B-lines, confluent B-lines, subpleural consolidation, the shred sign, to a dense consolidation. Once the air is completely gone from the lung and replaced with fluid this will result in an echogenic structure on ultrasound similar to echogenicity of the liver. This is termed “hepatization of the lung.”
Here is an example of subpleural consolidation:
The Shred sign
The border at which the fluid or pus-filled lung tissue meets air looks like a jagged echoic edge which is known as the “Shred sign” shown below (Lichtenstein 2009).
Dense Lung Consolidation
When lung is completely filled with fluid or is completely collapsed (atelectasis) you will have a dense appearing lung consolidation (Hepatization of the lung)
Air Bronchograms
Consolidations can also present with static and/or dynamic air bronchograms. On ultrasound, this trapped air appears as small hyperechoic specks.
- Dynamic Air Bronchograms tend to occur in pneumonia and move as the patient inhales and exhales.
- Static Air Bronchograms tend to occur when air bubbles are trapped behind an obstruction, as occurs in atelectasis, and don’t move with respiration.
Pleural Effusions
Pleural effusions occur when transudate or exudate builds up in the base of the lungs. They are best viewed from the PLAPS-point where the lower lobes are viewed. Point of Care Ultrasound (POCUS) is over 90% sensitive and specific for the detection of pleural effusions.
In this section you will learn how to recognize pleural effusions, calculate pleural effusion size, look for all of the common ultrasound signs.
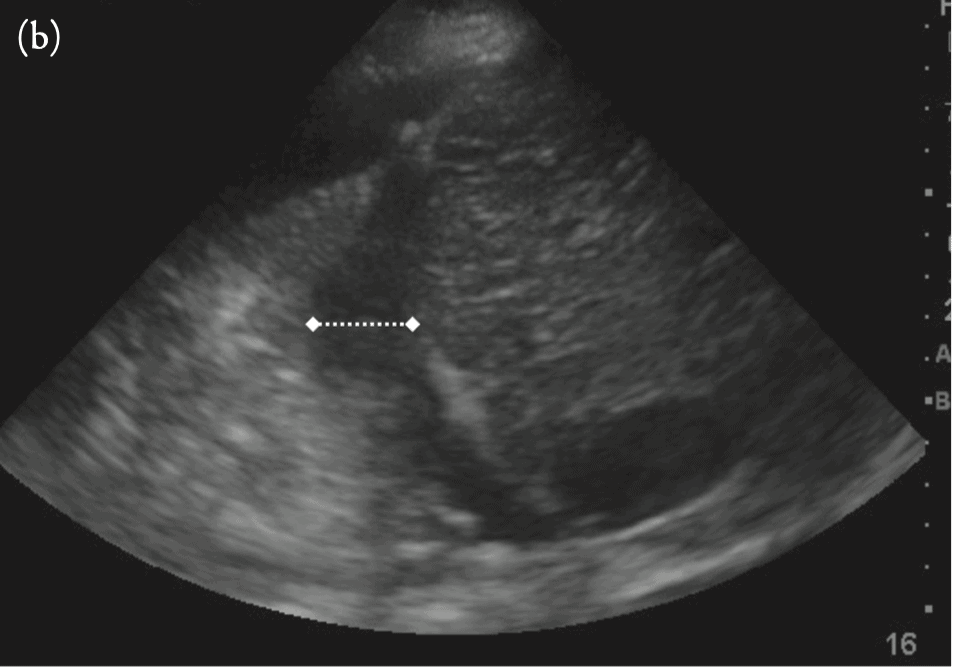
Calculating Pleural Effusion Size
The simplest way to estimate pleural effusion volume is to use the formula by Balik et al. It involves measuring the maximal effusion diameter ( in millimeters) between the diaphragm and base of the lung in a supine patient (see Figure Below) and multiplying that number by 20.
Pleural volume (mL) = (measured distance in mm) x 20.
Ultrasound Signs of Pleural Effusions
The PLAPS point is the most specific and sensitive view used to diagnose pleural effusion. If you have a patient with a suspected pleural effusion, the following signs/findings that can help you arrive at a proper diagnosis:
- Spine Sign
- Jellyfish sign
- Sinusoid Sign
- Quad Sign
- Plankton Sign
- Hematocrit Sign
- Loculated Pleural Effusions
Spine Sign
You will find a Spine sign at the PLAPS point along with a pleural effusion.
In a normal lung, you should be able to see the spine up until the edge of the diaphragm, but never passing the diaphragm. This is because the lung’s air above the diaphragm prevents any sound waves from passing.
However, in pleural effusions, sound waves can pass through the pleural fluid allowing the spine to be seen above the diaphragm.
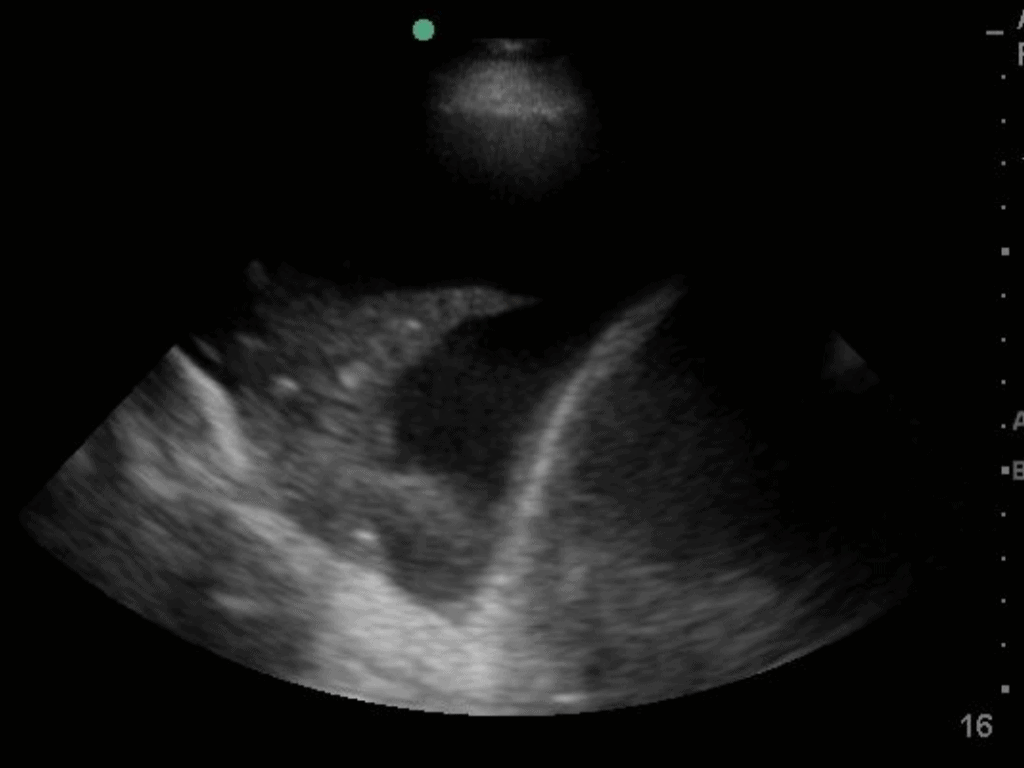
Jellyfish Sign
You will find the Jellyfish sign at the PLAPS-point, located slightly above the diaphragm, in the RUQ. Recall that the PLAPS-point is the key location to find pleural effusions. The “Jellyfish Sign” occurs when aconsolidated lung is seen floating in the pleural effusion.
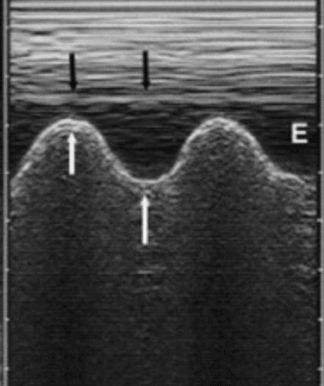
Sinusoid Sign
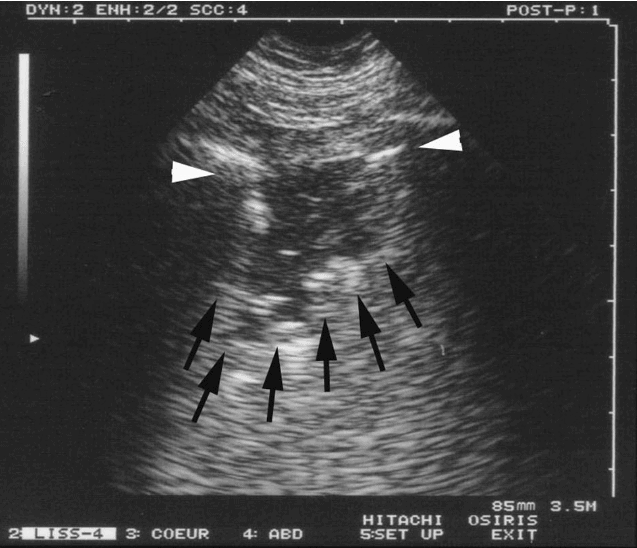
- You can turn on M-mode to look for the Sinusoid sign (looks like a sine wave). It is caused by the parietal and visceral pleura moving closer and further apart while the patient breathes. (White arrows point to the lung line/visceral pleura while black arrows point to the pleural line/parietal pleura). It is equivalent to an M-mode view of the jellyfish sign.
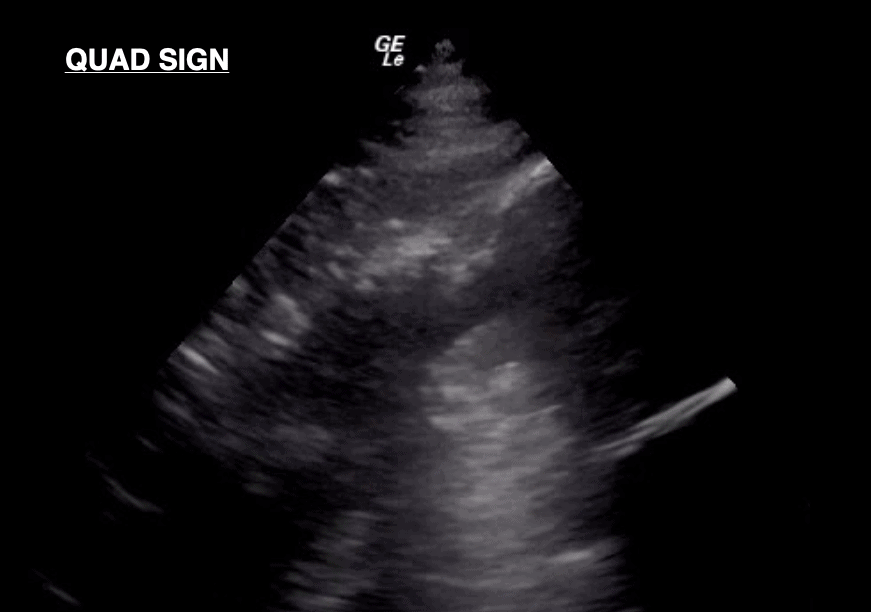
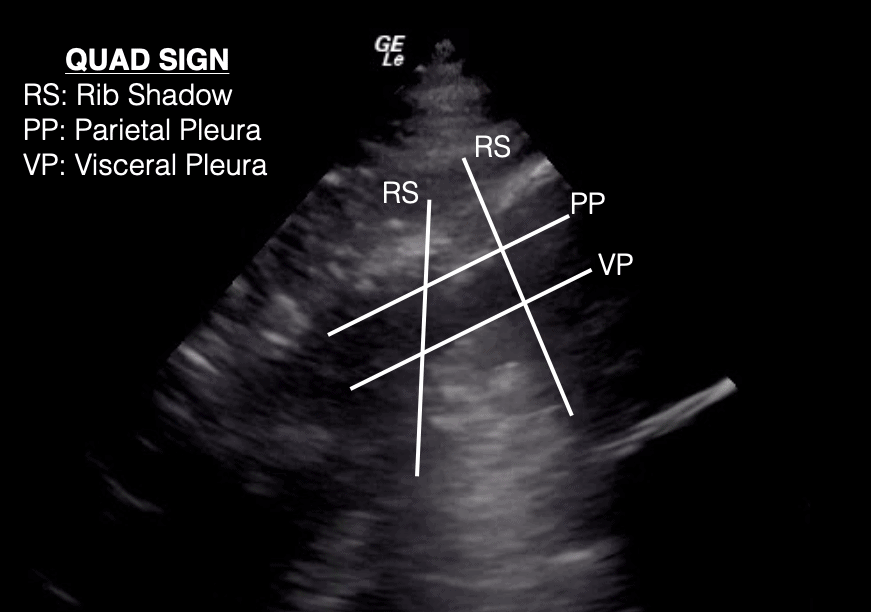
Quad Sign
- A pleural effusion has an anechoic appearance often delineated by the pleural line, the rib shadows, and the lung line, called the “Quad Sign.”
Plankton Sign
Now that you know how to detect a pleural effusion on point of care ultrasound (POCUS), you can further differentiate pleural effusions into transudative or exudative. Though most effusions are transudative, exudative effusions can have the plankton sign, as seen below. The plankton sign shows an effusion with swirling, hyperechoic debris.
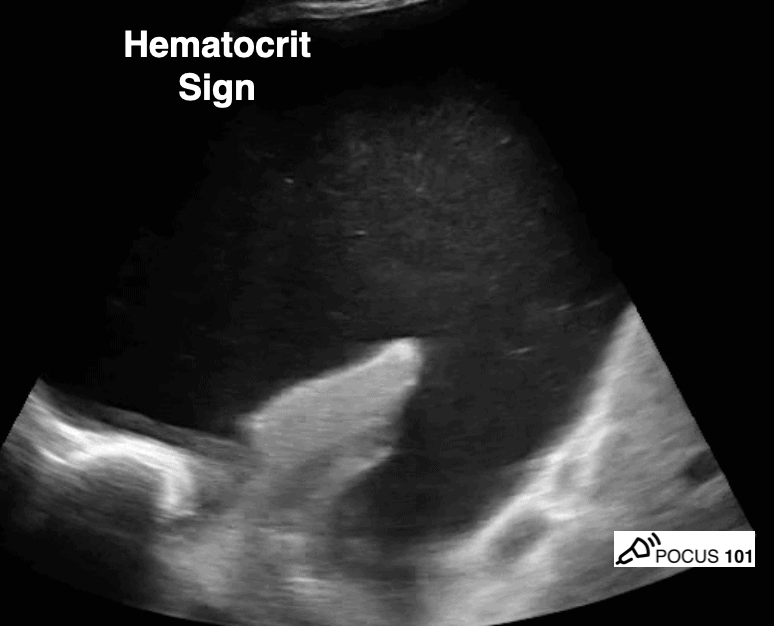
Hematocrit Sign
The hematocrit sign refers to the echogenic layering of material in a pleural effusion. This can be due to exudative effusions or a hemothorax (Chichra A).
Transudative vs Exudative Pleural Effusion
Here are some differences between transudative and exudative pleural effusions:
| Transudative Pleural Effusion | Exudative Pleural Effusion | |
| Ultrasound Findings | – Absent plankton sign/hematocrit sign – Typical effusion signs |
– Present plankton sign/hematocrit sign -Typical effusion signs |
| Fluid Quality | – Transudate withlowprotein and cell count – Normal glucose levels |
– Cloudy transudate with highprotein and cell count – Light’s Criteria: Pleural fluid protein >0.5 and LDH >0.6 or LDH – Low glucose levels |
| Mechanism | – Increased capillary hydrostatic pressure and/or decreased capillary oncotic pressure (low albumin). | – Increased vascular permeability from inflammation/infection/malignancy |
| Common Etiologies | – Heart failure, nephrotic syndrome, liver cirrhosis | – Trauma (hemothorax), bacterial infections, lymphatic obstructions, malignancies, pulmonary embolism |
Loculated Pleural Effusion
- Loculated (or septated) pleural effusions are most often seen in exudative effusions and describe any effusion with fluid divided into “pockets.” They can be caused by infections, abscesses, scarring, or fibrosis in the pleural cavity that complicates proper fluid drainage.
The image below shows an image of a loculated pleural effusion that lies above the diaphragm.
Major Lung Ultrasound Pathology Profiles
Now that you have a grasp of the most common pathological lung signs to look for, this section will help you use those findings to characterize more specifically the ultrasound profiles of pneumothorax, pneumonia, cardiogenic pulmonary edema, acute respiratory distress syndrome, and COPD.
You can choose to use an algorithm such as the Blue Protocol (Lichtenstein, et al) but after teaching many learners lung ultrasound we’ve found it much easier for you to recognize the lung ultrasound findings that go along with each disease pattern. We will present all of the major disease findings and give you examples of the corresponding lung ultrasound findings below.
Lung signs/findings specific to each disease will be further explained within their respective section. Keep in mind, these are the potential Lung ultrasound findings you will see at the bedside, however, you must coordinate these profiles clinically with what is going on with the patient.
| Pulmonary Pathology | Lung Ultrasound Findings |
| Pneumothorax | – No lung sliding/barcode sign – Lung point (hard to find) – Bilateral A-lines (parietal pleura reflection) |
| Pneumonia | – Consolidation or “hepatization of the lung” – Supleural Consolidations – “Shred” sign – Unilateral B-linesor bilateral B-lines – Possible small plural effusion – Reduced lung sliding due to thickened pleura in severe cases – Dynamic air bronchograms (atelectasis has static bronchograms) |
| Cardiogenic Pulmonary Edema | – Widespread and bilateral B-lines – Normal lung sliding – Possible bilateral effusion depending on the severity |
| Acute Respiratory Distress Syndrome (ARDS) | – Bilateral or unilateral B-lines – Normal lung sliding |
| COPD or Asthma | – Bilateral A-lines – Reduced lung sliding |
| Pulmonary Embolism (PE) | – Bilateral A-Lines – Deep Vein Thrombosis in Upper or Lower Extremities – Right Ventricular Enlargement (massive/submassive PE) |
Pneumothorax
Ultrasound is incredibly useful for diagnosing pneumothorax with high sensitivity and specificity. A pneumothorax occurs when a lung collapses due to loss of negative pressure between the visceral and parietal pleurae. This abolishes lung sliding.
However, there is usually a location where sliding still exists. The transition from sliding to no sliding is known as the lung point sign. Though difficult to find, a lung point is 100% specific for ruling in a pneumothorax (Chan S.).
Clinical manifestations of pneumothorax include pleuritic chest pain, dyspnea, tachycardia, and reduced breath sounds on the affected side.
Ultrasound Profile of Pneumothorax
- No lung sliding
- M-mode barcode sign
- Lung point Sign
- A-lines from intact parietal pleura
Here are three important steps to evaluating for pneumothorax:
First, if lung sliding is present, you can rule out pneumothorax with 100% accuracy at that ultrasound point (Husain LF).
Remember that presence of lung sliding only rules out pneumothorax at that specific point you are scanning. Make sure to maximize your sensitivity by scanning multiple points on the chest.
You can look for lung sliding with B-mode or M-mode:
Second, if lung sliding is ABSENT, you should not automatically assume pneumothorax.
Recall other causes of reduced/absent lung sliding: severe consolidation, chemical pleurodesis, acute infectious or inflammatory states, fibrotic lung diseases, acute respiratory distress syndrome, or mainstem intubation.
Third, if a lung point is present, you can rule in pneumothorax with 100% accuracy (Chan S).
To confirm the presence of a pneumothorax, you should look for the “Lung Point Sign.“
The lung point is when you can see the transition between normal lung sliding and the absence of lung sliding. This is the transition point between the collapsed lung and normal lung. If you see this you can definitively rule in a pneumothorax. The Lung point sign also helps you quantify how large a pneumothorax is.
If you think you may have found a lung point but are not sure, use M-Mode and place your cursor at the intersection where you think lung sliding starts and stops. If you see a normal seashore sign that turns into an abnormal barcode sign, then you have located the lung point with M-Mode.
Pneumonia
Pneumonia is an infection that inflames the alveoli and fills them with fluid. This extra fluid creates unilateral or bilateral B-lines depending if one or both lungs are affected.
The fluid or pus-filled alveoli also cause a productive cough with colored phlegm, fever, chills, and difficulty breathing.
Ultrasound Profile of Pneumonia:
- Shred sign
- Consolidated lung tissue with dynamic air bronchograms
- B-lines: unilateral (bacterial) or bilateral (viral)
- Decreased lung sliding depending on severity
- Small pleural effusion depending on severity
Even the most experienced ultrasound practitioners have difficulty distinguishing pneumonia from atelectasis using ultrasound alone. Thus, a clear clinical picture is necessary before determining the true cause of lung consolidation. The table below outlines some of the key differentiatingfactors between pneumonia and atelectasis.
| Pneumonia | Atelectasis | |
| US Findings | – Consolidation pattern – Shred sign – Dynamic bronchograms – Possible pleural effusion (parapneumonic effusion) |
– Consolidation pattern – Static air bronchograms |
| Distinguishing clinical features | – Fever and chills – Cough with colored mucous or blood – Severe Malaise – Crackles and breath sounds |
– Obstruction to airway – Acute dyspnea – Mucous plug in Bronchus |
Cardiogenic Pulmonary Edema (CPE)
Ultrasound is useful for assessing the severity of cardiogenic pulmonary edema. Cardiogenic pulmonary edema is a type of pulmonary edema caused by increased pressures of the left side of the heart. This condition often occurs secondary to congestive heart failure when the left ventricle cannot pump out all the blood it receives from the lungs. The backed-up blood increases capillary hydrostatic pressure that then causes fluid to leak into both lungs, resulting in bilateral and symmetric B-lines.
As CPE progresses, more B-lines appear until they converge into vertical sheets, known as confluent B-lines. As fluid builds up further, expect to see bilateral transudative pleural effusions with atelectasis of the lungs. Cardiogenic pulmonary edema usually affects both lungs but can atypically affect a unilateral lung.
If you suspect your patient has CPE, it is also recommended to perform an ultrasound evaluation of their heart to assess for systolic and diastolic dysfunction of the left ventricle.
Cardiogenic Pulmonary Edema – Lung Ultrasound Profile:
- Bilateral and Symmetric B-lines (can sometimes be unilateral)
- Confluent B-lines with increasing severity
- Pleural edema and/or bilateral effusions with increasing severity
- Lung Sliding Present
Acute Respiratory Distress Syndrome
Acute respiratory distress syndrome (ARDS) is often fatal and the risk of death increases with age and severity of the illness. ARDS is characterized by the rapid onset of widespread inflammation in the lungs. The most common cause of ARDS is sepsis, but can also be precipitated by inhalation of harmful substances, pancreatitis, aspiration, severe pneumonia, or near-drowning experiences. Notice how nearly all of these etiologies involve a form of fluid buildup or inflammation so ARDS will present with B-lines on thoracic ultrasound.
People with ARDS also have severe shortness of breath, rapid breathing, and may often need support from a ventilator.
Since the following ultrasound profile is similar to the profile of cardiogenic pulmonary edema, practitioners must use other clinical features to interpret these findings to rule out elevated left heart pressure as the cause of the B-lines.
ARDS Ultrasound Profile
- Bilateral or unilateral B-lines
- Lung sliding present (but may be diminished due to inflammation
- On echocardiography, the patient should have normal diastolic function.
Chronic Obstructive Pulmonary Disease/Asthma
Chronic obstructive pulmonary disease (COPD) is a collection of lung diseases that obstruct airflow. This group of diseases can include asthma, emphysema, and chronic bronchitis. Patients with COPD or severe asthma often have hyperinflated lungs. If hyperinflation is severe enough, the resultant shallow breathing can reduce lung sliding.
If you see normal findings such as lung sliding and A-lines but the patient still has symptoms and difficulty breathing, you should consider COPD, asthma, pulmonary embolism, or nonpulmonary conditions causing the patient’s dyspnea.
COPD/Asthma Ultrasound Profile
- Bilateral A-lines
- Normal sliding or reduced lung sliding (as seen in severe asthma/COPD)
Pulmonary Embolism
Pulmonary embolism is often a difficult and missed diagnosis. Unfortunately lung ultrasound will usually appear normal (lung sliding with A-lines) in patients with pulmonary embolism.
If you are concerned for pulmonary embolism, perform a cardiac ultrasound to look for right ventricular strain and a lower extremity DVT (deep vein thrombosis) scan rule out venous thromboemolism. If those ultrasounds are normal consider obtaining a CT angiogram of the chest to look for pulmonary embolism.
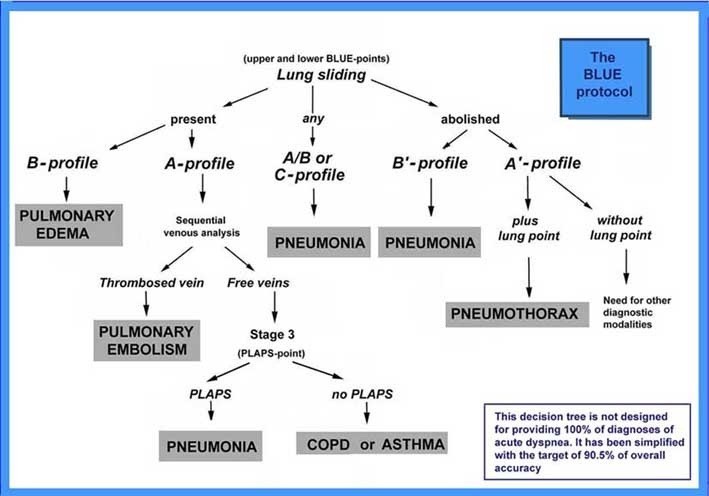
The Blue Protocol
Researchers have created protocols to streamline the use of pulmonary ultrasound in clinical practice. The most widely used protocol has been the BLUE protocol created by Lichenstein and colleagues and is used by many practitioners to diagnose the cause of acute respiratory failure. Pulmonary edema, pulmonary embolism, pneumonia, chronic obstructive pulmonary disease, asthma, and pneumothorax yield specific profiles predicted by the BLUE protocol.
This protocol classifies A-lines and B-lines into various profiles. Though quite simple, they can be confusing if you are not first familiar with them.
- “A-profile” has A-lines with lung sliding and describes normal lungs
- “B-profile” has B-lines and lung sliding
- “B’ profile” has B-lines with impaired lung sliding
- “A’ profile” has A-lines with impaired lung sliding
- A/B profile has one lung with A-lines and the other with B-lines.
References
- Biswas, A., Lascano, J. E., Mehta, H. J., & Faruqi, I. (2017). The Utility of the “Shred Sign” in the Diagnosis of Acute Respiratory Distress Syndrome Resulting from Multifocal Pneumonia. American Journal of Respiratory and Critical Care Medicine, 195(2). doi:10.1164/rccm.201608-1671im
- Chan S. Emergency Bedside Ultrasound to Detect Pneumothorax. Acad Emerg Med January 2003.
- Chichra, A., Makaryus, M., Chaudhri, P., & Narasimhan, M. (2016). Ultrasound for the Pulmonary Consultant. Clinical medicine insights. Circulatory, respiratory and pulmonary medicine, 10, 1–9. https://doi.org/10.4137/CCRPM.S33382
- Dwyer, Kristin & Rempell, Joshua. (2016). Young Woman with a Fever and Chest Pain. Western Journal of Emergency Medicine. 17. 186-187. 10.5811/westjem.2016.1.29233.
- Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134:117–125.
- Lichtenstein, D., Mezière, G., Seitz, J. (2009). The dynamic air bronchogram. A lung ultrasound sign of alveolar consolidation ruling out atelectasis. Chest 135(6), 1421 – 1425. https://dx.doi.org/10.1378/chest.08-2281
- Lichtenstein DA, Lascols N, Mezière G, et al. Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med. 2004;30:276–281.
- Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9 –15.
- Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensive Care. 2014;4(1):1. Published 2014 Jan 9. doi:10.1186/2110-5820-4-1
- Lobo, Viveta & Hunter-Behrend, Michelle & Cullnan, Erin & Higbee, Rebecca & Phillips, Caleb & Williams, Sarah & Perera, Philips & Gharahbaghian, Laleh. (2017). Caudal Edge of the Liver in the Right Upper Quadrant (RUQ) View Is the Most Sensitive Area for Free Fluid on the FAST Exam. Western Journal of Emergency Medicine. 18. 270-280. 10.5811/westjem.2016.11.30435.
- Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012;5(1):76-81. doi:10.4103/0974-2700.93116
- Soni NJ, Franco R, Velez MI, et al. Ultrasound in the diagnosis and management of pleural effusions. J Hosp Med. 2015;10(12):811-816. doi:10.1002/jhm.2434
- Rocco M, Carbone I, Morelli A, et al. Diagnostic accuracy of bedside ultrasonography in the ICU: feasibility of detecting pulmonary effusion and lung contusion in patients on respiratory support after severe blunt thoracic trauma. Acta anaesthesiologica Scandinavica. 2008;52(6):776–784.
- Volpicelli G, Caramello V, Cardinale L, Cravino M. Diagnosis of radio-occult pulmonary conditions by real-time chest ultrasonography in patients with pleuritic pain. Ultrasound Med Biol. 2008;34(11):1717-1723. doi:10.1016/j.ultrasmedbio.2008.04.00
- Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9 [PubMed] [Google Scholar]
- 19. Grimberg A, Shigueoka DC, Atallah AN, Ajzen S, Iared W. Diagnostic accuracy of sonography for pleural effusion: systematic review. Sao Paulo Med J. 2010;128(2):90–95. [PubMed] [Google Scholar]
- Kataoka H, Takada S. The role of thoracic ultrasonography for evaluation of patients with decompensated chronic heart failure. Journal of the American College of Cardiology. 2000;35(6):1638–1646. [PubMed] [Google Scholar]21. Ma OJ, Mateer JR. Trauma ultrasound examination versus chest radiography in the detection of hemothorax. Annals of emergency medicine. 1997;29(3):312–315. discussion 315-316. [PubMed] [Google Scholar]